It’s Diabetic Eye Disease Awareness Month: What You Should Know
Many people know that diabetes can seriously impact a person’s blood pressure, heart health and stroke risk, but not everyone realizes that the disease is just as perilous for the eyes. Diabetic eye disease is the No. 1 cause of new blindness in adults in the United States. If you have diabetes, you are more likely to develop glaucoma, cataracts and diabetic retinopathy.
November is Diabetic Eye Disease Awareness Month, and our eye doctors at Mittleman Eye aim to help spread the word about vision loss and blindness due to diabetes.
What is Diabetic Retinopathy?
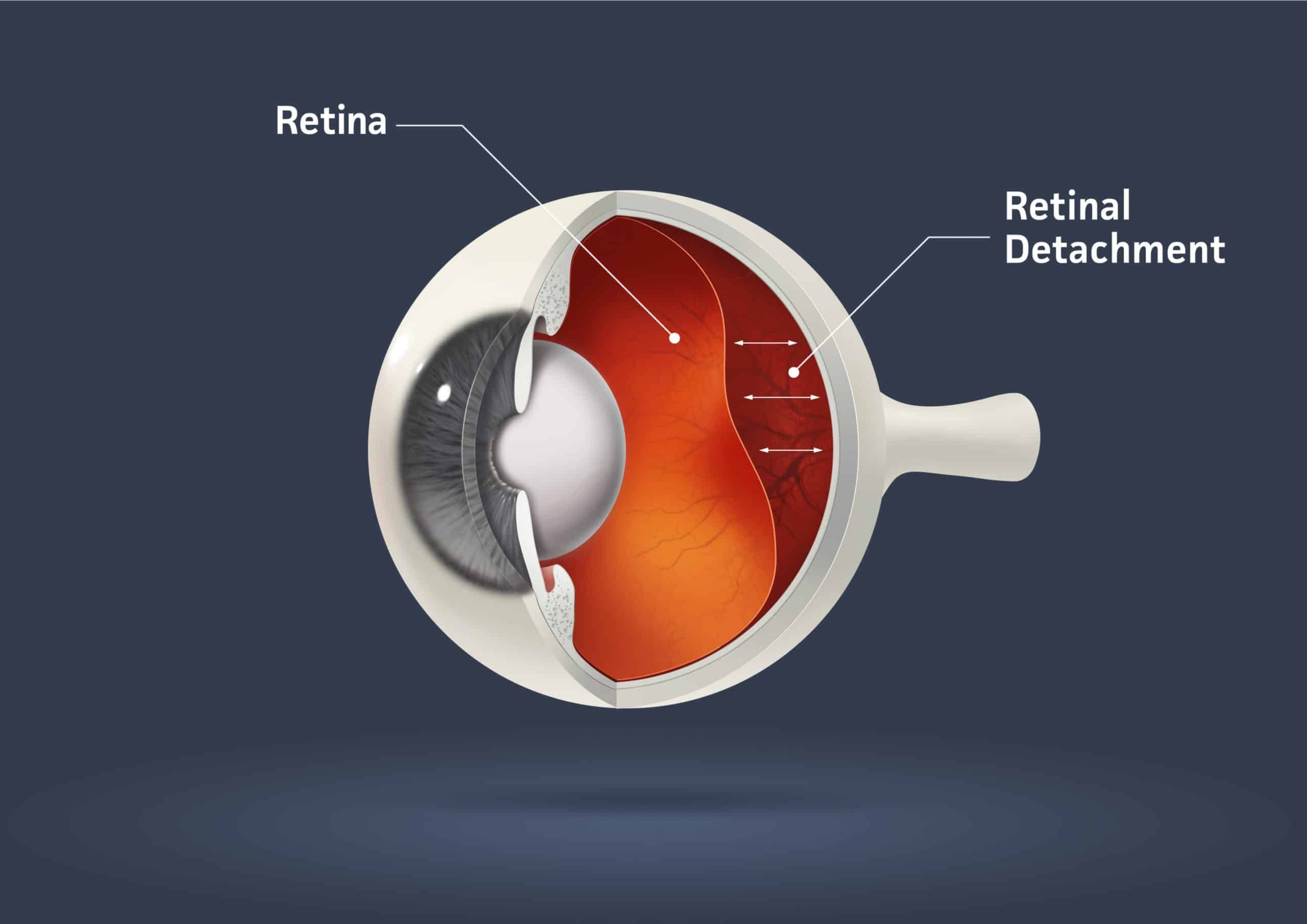
The inside surface of your eye is lined with a thin, light-sensitive tissue called the retina. Nerve cells in the retina convert light to electrical impulses that are sent to the brain via the optic nerve and translated into images. The nerve cells and tissues in the retina rely on nourishment from tiny blood vessels. In diabetic people, too-high blood sugar levels cause those blood vessels to leak, swell or cease functioning altogether, a condition known as diabetic retinopathy.
The late stage of diabetic retinopathy causes new blood vessels to grow and leak into the eye’s vitreous fluid. These new vessels may form scar tissue, leading to a detached retina and ultimately causing partial or complete blindness. That abnormal blood vessel growth is called proliferative diabetic retinopathy and affects about 1 in 20 people living with the condition.
What is Diabetic Macular Edema?
The macula is part of your retina located at the back of your eye and is responsible for your central vision. Macular edema occurs when those swelling blood vessels leak into the macula, causing it to thicken, swell and distort your vision. That may not always lead to blindness or severe vision loss, but it can significantly impact your central vision or ability to see details. Diabetic macular edema is a common problem as diabetic retinopathy progresses.
It’s unlikely you will experience symptoms during the early stages of diabetic retinopathy. The late stages of the disease may cause these vision changes:
- Sudden onset of eye floaters
- Blurry vision
- Rapid vision loss in one eye
- Flashes of light
- Poor night or color vision
- Light halos
Are You at Risk for Diabetic Eye Disease?
People living with uncontrolled diabetes are at high risk for diabetic eye disease. Other factors that may increase your likelihood of retina damage and vision loss include:
- Long-term diabetes
- Poor management of blood glucose
- Smoking
- High blood pressure and cholesterol
- Pregnancy
- Kidney disease
The only way to diagnose diabetic retinopathy early is through regular comprehensive eye examinations that search for indications of the disease in diabetic patients.
Treatments for Diabetic Eye Disease
Our ophthalmologists treat eye diseases that often affect people with diabetes. We believe one of the best treatments is to address the root of the problem — appropriate diabetes management by taking your medications correctly, seeing your medical team often and living a healthy lifestyle with a high-fiber diet and exercise. Diabetic retinopathy can be treated with surgery or injected medications such as Avastin, Eylea, and Lucentis or steroids.
Celebrate Diabetic Eye Disease Awareness Month with an Eye Exam
Our eye doctors recommend annual eye examinations, but those living with diabetes may need to visit Mittleman Eye more often to detect diabetic eye disease early. In celebration of Diabetic Eye Disease Awareness Month, call or text (561) 500-2020 to schedule your eye exam online today.